Procedures & Surgeries
Advanced office-based and operating room interventions provided at New England Retina Care
Intravitreal Injections
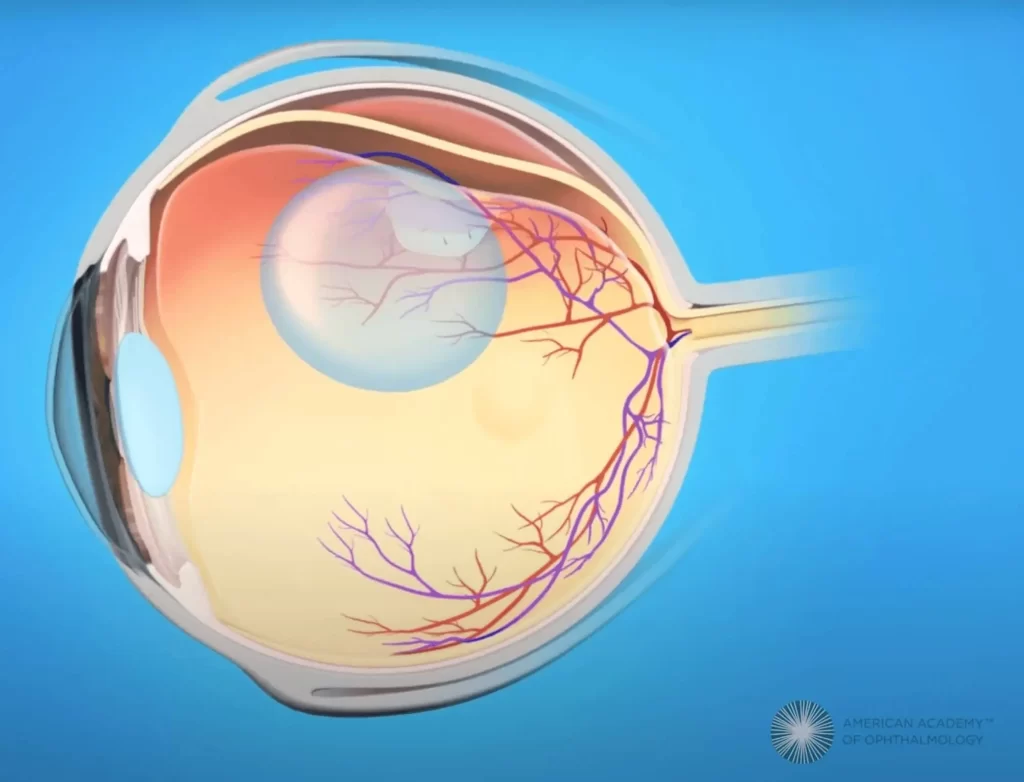
The advent of intravitreal injections has revolutionized the landscape of vitreoretinal surgery by offering a minimally invasive yet highly effective treatment for a wide range of retinal conditions. Administered directly into the vitreous, the gel-like substance in the center of the eye, these injections deliver medication to target specific disorders. The primary purpose of intravitreal injections is to manage conditions such as age-related macular degeneration (AMD), diabetic retinopathy macular edema, and retinal vein occlusion.
Before the procedure, the eye is numbed with local anesthesia to minimize discomfort. The patient may experience slight pressure or a brief sting during the injection, but it is typically well-tolerated. Following the injection, the patient is monitored for a short period to check for any immediate side effects or complications. Recovery time is usually quick, and patients can resume normal activities soon after the procedure.
Though generally safe, intravitreal injections carry some risks, including infection, bleeding, elevated intraocular pressure, and retinal detachment. Patients are advised to promptly report any sudden changes in vision, pain, or discomfort after the procedure.

Retina Laser Treatment
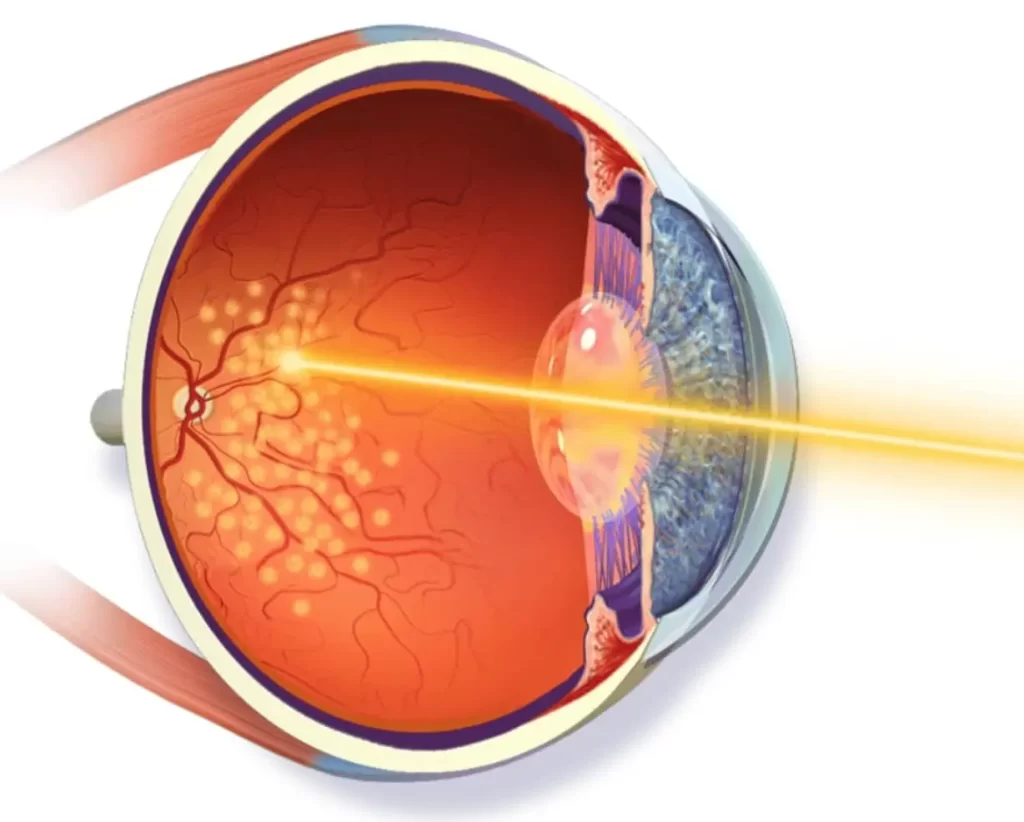
Retina Laser Treatment, also known as Laser Photocoagulation, is a therapeutic procedure used to treat various retinal conditions by utilizing a focused laser beam. This treatment aims to prevent or slow down the progression of disorders such as diabetic retinopathy, retinal tears, macular edema, and certain types of retinal detachments.
The process involves a specialized laser that emits a precisely concentrated beam of light, which is directed into the eye through a contact lens or ophthalmoscope. The laser energy is absorbed by the targeted tissues in the retina, causing photocoagulation and sealing off abnormal blood vessels or repairing retinal tears. For diabetic retinopathy, the laser helps to reduce swelling and to prevent growth of new, fragile blood vessels that lead to vision loss.
Retina Laser Treatment is typically performed in an outpatient setting and is often well-tolerated by patients. Local anesthesia may be applied to numb the eye, and the procedure itself can range from a few minutes to around an hour, depending on the complexity and extent of the condition being treated. Post-treatment, patients might experience mild discomfort, blurred vision, or sensitivity to light for a short period. Recovery time is usually quick, and patients can resume normal activities soon after the procedure.
Cryopexy
Cryopexy is a specialized technique in ophthalmology used to treat certain retinal conditions by applying freezing energy to specific areas of the retina. This procedure is particularly employed to repair retinal tears or detachments. By using extreme cold temperatures, cryopexy creates controlled tissue adhesion, essentially sealing the tear and preventing further detachment.
Cryopexy is often performed in an outpatient setting and may involve local anesthesia to numb the eye, ensuring patient comfort during the procedure. The duration of the treatment depends on the location and size of the retinal tear being treated. Post-cryopexy, patients might experience mild discomfort, redness, or blurry vision for a short period. Recovery time is typically rapid, and patients can usually resume normal activities soon after the procedure.
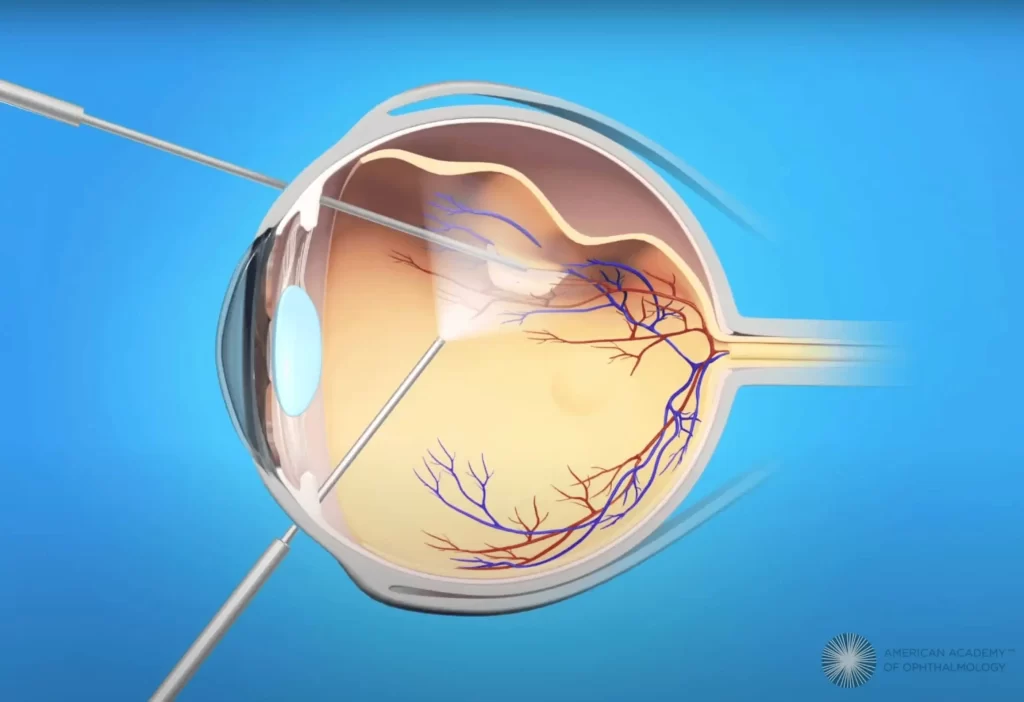
Vitrectomy
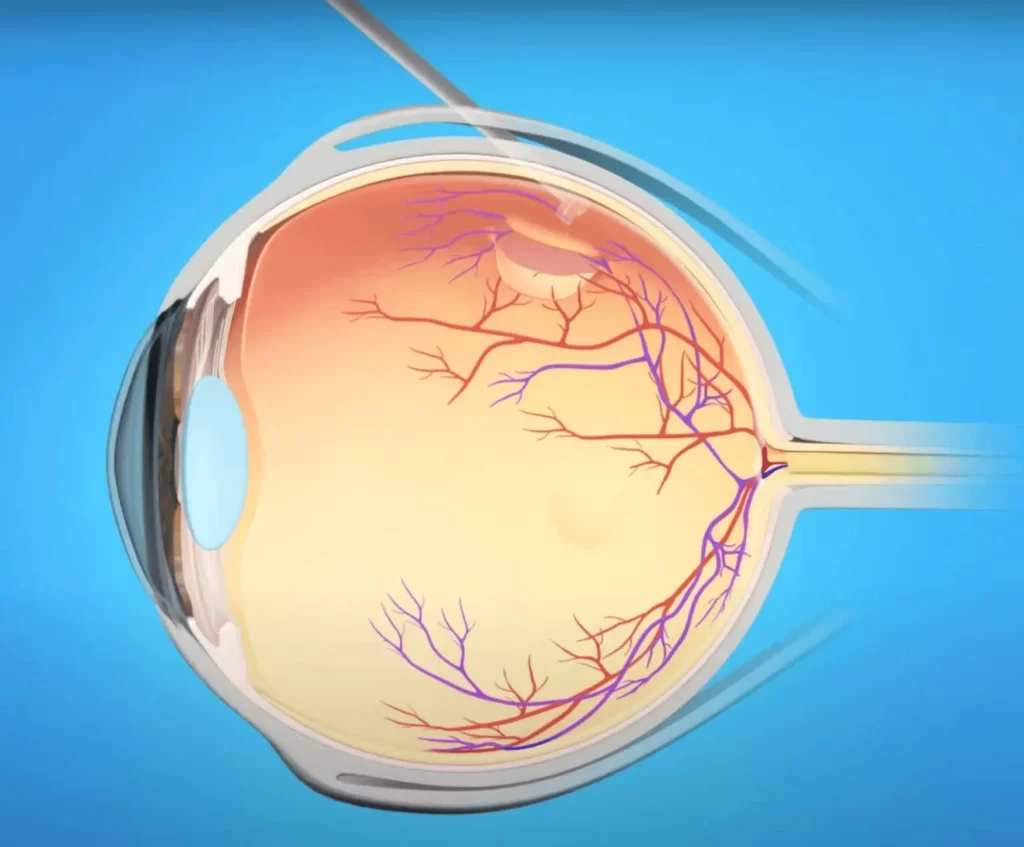
Vitrectomy is a sophisticated surgical procedure performed by a vitreoretinal surgeon to address a wide range of eye conditions affecting the vitreous humor and the retina. This surgery is conducted using microsurgical instruments inserted through small incisions in the eye and is used for management a wide range of retinal conditions including retinal detachment, vitreous floaters, macular hole, and dislocated intraocular lens.
During vitrectomy, a small probe or cutter, is entered the eye to carefully remove the vitreous gel while maintaining the eye’s shape and structure. Once the vitreous gel is removed, the surgeon can perform additional procedures to repair retinal detachments, remove scar tissue, or address other conditions affecting the retina. Vitrectomy procedures are tailored to each patient’s specific eye condition and can vary in complexity and duration. Some surgeries may be completed within an hour, while others might require a more extended period in the operating room.
After vitrectomy, patients may experience temporary discomfort, redness, or blurred vision. Recovery times vary depending on the complexity of the surgery and the individual’s overall eye health. Patients are typically advised to avoid strenuous activities, keep the eye protected, and adhere to a prescribed regimen of eye drops to prevent infection and promote healing.
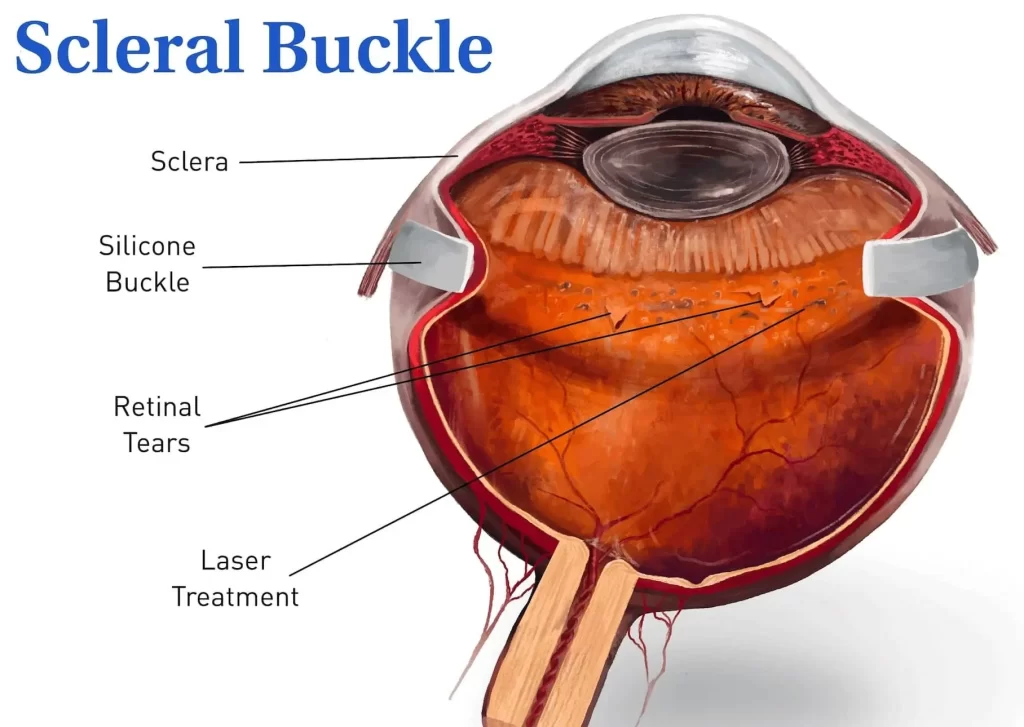
Scleral Buckle
Scleral buckle surgery is a specialized procedure primarily used to treat retinal detachments. This surgical procedure which predates vitrectomy, was first introduced in mid-20th century as a primary treatment for retinal detachment. While less widely used after the advent of vitrectomy, scleral buckle is still utilized for repair of certain types of retinal detachment.
This surgical technique involves placing a flexible band, made of silicone or other materials, around the eye to support and reattach the retina. During scleral buckle surgery, the vitreoretinal surgeon makes small incisions in the eye’s outer layer, the sclera, and carefully positions the buckle element against the affected area of the retina. The buckle exerts gentle external pressure on the eye, counteracting the forces pulling the retina away from the underlying tissue. This pressure helps the retina reattach and remain in place, allowing the retinal tissue to heal. In some cases, vitrectomy may be performed in conjunction with the placement of the scleral buckle to further secure the retina in its proper position.
Pneumatic Retinopexy
Pneumatic Retinopexy is an officed-based surgical procedure used to repair certain types of retinal detachments. Unlike more traditional retinal detachment surgeries, pneumatic retinopexy is often performed in an outpatient setting without the need for extensive incisions or general anesthesia. This procedure involves injecting a small gas bubble into the vitreous cavity of the eye. The gas bubble is carefully positioned to push against the detached retina, sealing the retinal tear or hole. To aid in the reattachment process, the surgeon may also use cryopexy or laser therapy to create scars around the tear, ensuring a secure bond between the retina and the underlying tissue.
Once the gas bubble is in place, the patient’s head is positioned strategically to allow the bubble to float and cover the affected area of the retina. Patients are instructed to maintain a specific head position for a period following the procedure to keep the gas bubble in the optimal position for effective retinal reattachment. Over time, the body naturally absorbs the gas bubble, and as the bubble diminishes in size, the retina heals and reattaches to the eye wall.